Suboxone Detox: Signs, Symptoms, and How to Taper Off
Suboxone is often prescribed as part of medication-assisted treatment for opioid dependence. It serves a crucial role in alleviating withdrawal symptoms and reducing cravings, allowing people to stabilize their lives and begin the journey towards recovery. However, like many medications, Suboxone also carries the potential for abuse when used improperly.[1]
For those seeking to break free from opioid addiction, detoxification from Suboxone can be a challenging step. Unlike abrupt cessation, a carefully managed tapering process under medical supervision is typically recommended to minimize withdrawal symptoms and ensure your safety.
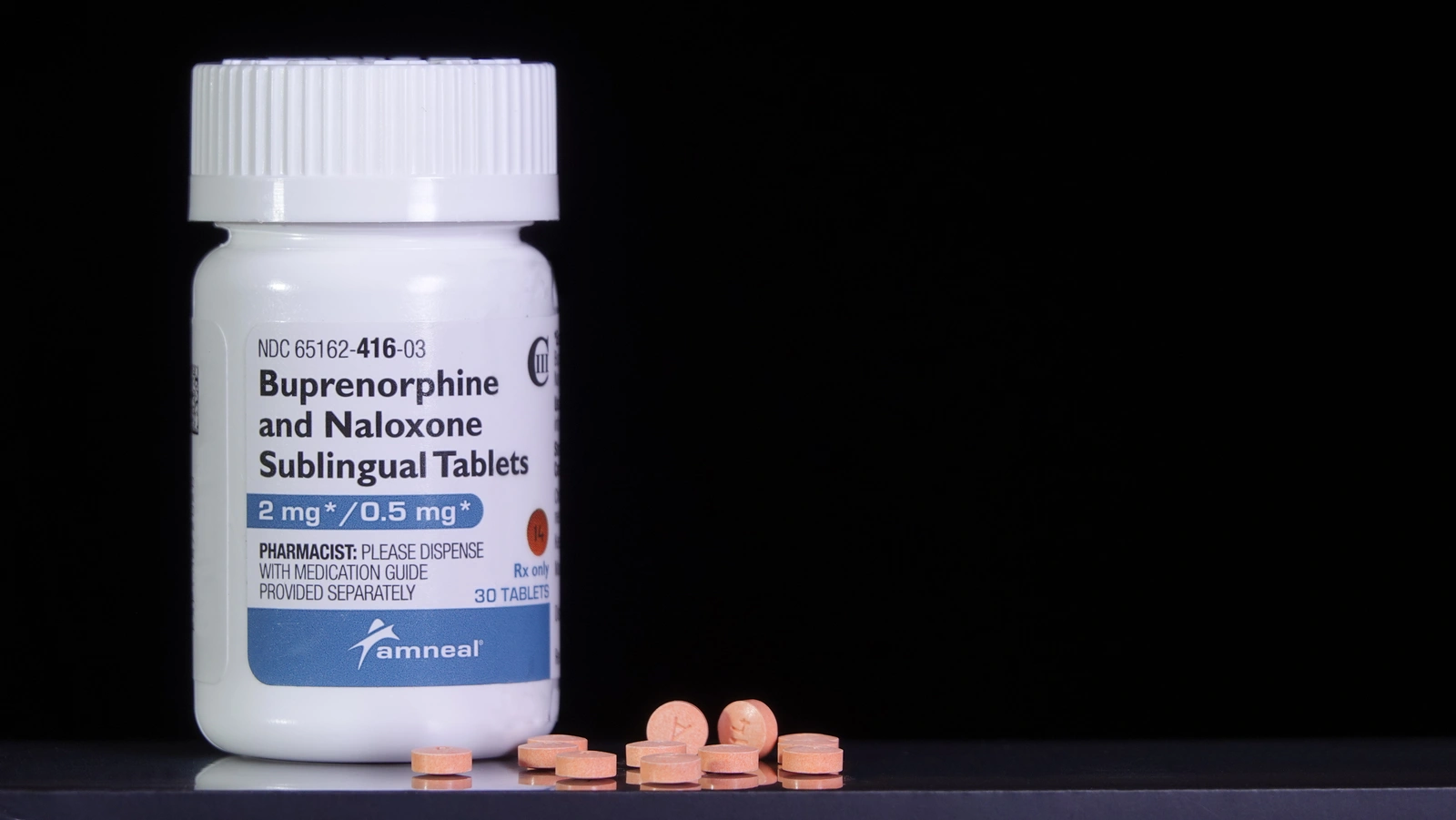
- Suboxone is a combination medication used to treat opioid dependence, comprised of buprenorphine and naloxone.
- Despite its therapeutic benefits, Suboxone carries the risk of addiction and misuse, leading to physical dependence and withdrawal symptoms if not used as prescribed.
- Weaning off Suboxone without treatment is not recommended due to the severity of withdrawal symptoms, complexity of tapering, increased risk of relapse, lack of support, and potential underlying issues.
- Treatment options for Suboxone abuse and addiction include detoxification, residential treatment, family programs, discharge planning, and various therapeutic modalities like ACT, art therapy, CBT, and DBT.
What is Suboxone?
Suboxone is a prescription medication used in the treatment of opioid dependence and addiction. It is a combination of two active ingredients: buprenorphine and naloxone.[2]
Buprenorphine is a partial opioid agonist, meaning it activates the same receptors in the brain that opioids do, but to a lesser extent.[3] This helps to reduce cravings and withdrawal symptoms without producing the intense euphoria associated with full opioid agonists like heroin or oxycodone. Naloxone, on the other hand, is an opioid antagonist, which blocks the effects of opioids and is included in Suboxone to deter misuse.[4]
Suboxone is typically administered as a sublingual film or tablet dissolved under the tongue. It is often used as part of a comprehensive treatment program that includes counseling and behavioral therapy to support people in their recovery journey. By alleviating withdrawal symptoms and reducing cravings, Suboxone can help people stabilize their lives and work towards long-term recovery from opioid addiction – but it can also be misused.
Suboxone Addiction and Abuse
Despite its potential benefits in treating opioid dependence, Suboxone carries the risk of addiction and abuse:[5]
Misuse and dependency:
While Suboxone is intended to aid in recovery by reducing withdrawal symptoms and cravings, some may misuse it for non-medical purposes. This can involve taking larger doses than prescribed, using it more frequently than directed, or using it without a prescription. Over time, this misuse can lead to physical dependence and addiction, as the body becomes reliant on the medication to function normally.
Risk Factors:
Several factors can increase the likelihood of Suboxone addiction and abuse, including a history of substance abuse, mental health disorders, genetic predisposition, and environmental influences.
Tolerance and withdrawal:
Prolonged use of Suboxone can lead to the development of tolerance, requiring higher doses to achieve the same effects. When people attempt to stop or reduce their use of Suboxone, they may experience opioid withdrawal symptoms and side effects, such as nausea, vomiting, diarrhea, muscle aches, anxiety, and insomnia.
Combination with other substances:
Suboxone misuse is often associated with the simultaneous use of other substances, such as alcohol, benzodiazepines, or illicit opioids. This polydrug use can increase the risk of overdose and other adverse health effects.
Opioid Addiction
Suboxone Quick Reference Chart
Drug Category
Commercial & Street Names
DEA Schedule
Administration
Is It Possible to Wean Off Suboxone Without Treatment?
Attempting to wean off Suboxone without treatment is generally not recommended, especially for those with a history of opioid dependence. Suboxone withdrawal can be challenging to manage without medical supervision and support, increasing the risk of relapse and other adverse outcomes:[6]
Risk of withdrawal symptoms:
Suboxone withdrawal symptoms can be severe and include nausea, vomiting, diarrhea, muscle aches, anxiety, insomnia, and intense cravings. Without medical detox, managing these symptoms can be difficult and may lead to a relapse.

The complexity of tapering:
Tapering off Suboxone requires a gradual reduction in dosage over an extended period to minimize withdrawal symptoms. Developing an appropriate tapering plan tailored to your individual needs requires medical expertise and monitoring.
Increased risk of relapse:
Weaning off Suboxone without treatment may increase the risk of relapse, as you may struggle to cope with cravings and withdrawal symptoms on your own. Relapse can derail progress and make it harder to achieve sustained recovery.
Lack of support:
Formal treatment programs offer comprehensive support and resources, including counseling, therapy, and medication management, that can greatly enhance the likelihood of successful recovery.
Underlying issues and dual diagnosis:
Tapering off Suboxone may uncover underlying issues contributing to opioid dependence, such as mental health disorders or unresolved trauma. Without professional support, addressing these issues may be challenging and could hinder long-term recovery efforts.

What Are My Treatment Options for Suboxone Abuse and Addiction?
Suboxone rehabilitation encompasses a comprehensive array of strategies tailored to address the intricate physical, psychological, and social dimensions of addiction. These treatment options span different levels of care and therapeutic modalities:
Levels of Care
Therapeutic Modalities
Frequently Asked Questions About Suboxone Detox and Treatment
What are the common withdrawal symptoms during Suboxone detox?
During Suboxone detox, common withdrawal symptoms may include nausea, vomiting, diarrhea, muscle aches, anxiety, insomnia, and cravings for opioids. These symptoms can vary in intensity depending on factors such as your individual dose, duration of Suboxone use, and overall health.
What is the difference between tapering off Suboxone and quitting cold turkey?
Tapering off Suboxone involves gradually reducing the dosage over a period of time to minimize withdrawal symptoms and allow the body to adjust to lower levels of the medication. Quitting cold turkey, on the other hand, involves abruptly stopping Suboxone without tapering, which can lead to more severe withdrawal symptoms and increase the risk of relapse.
Is Suboxone detox covered by insurance?
What aftercare support and discharge planning are available following Suboxone detox?
Following Suboxone detox, aftercare support may include outpatient therapy, support groups, and continued treatment engagement. These resources can help individuals maintain sobriety, address underlying issues contributing to addiction, and prevent relapse.
Sources
[1] Department of Justice. (n.d.). BULLETIN INTELLIGENCE. https://www.justice.gov/archive/ndic/pubs10/10123/10123p.pdf on June 5, 2024
[2] Substance Abuse and Mental Health Services Administration. (2023). Buprenorphine. Www.samhsa.gov. https://www.samhsa.gov/medications-substance-use-disorders/medications-counseling-related-conditions/buprenorphine on June 5, 2024
[3] Substance Abuse and Mental Health Services Administration. (2023). Buprenorphine. Www.samhsa.gov. https://www.samhsa.gov/medications-substance-use-disorders/medications-counseling-related-conditions/buprenorphine on June 5, 2024
[4] National Institute on Drug Abuse. (2022, January 11). Naloxone drug facts. National Institute on Drug Abuse. https://nida.nih.gov/publications/drugfacts/naloxone on June 5, 2024
[5] Suboxone addiction: Signs, withdrawal, treatment, more. (2022, May 31). Www.medicalnewstoday.com. https://www.medicalnewstoday.com/articles/is-suboxone-addictive on June 5, 2024
[6] Ling, W., Hillhouse, M., Domier, C., Doraimani, G., Hunter, J., Thomas, C., Jenkins, J., Hasson, A., Annon, J., Saxon, A., Selzer, J., Boverman, J., & Bilangi, R. (2009). Buprenorphine tapering schedule and illicit opioid use. Addiction (Abingdon, England), 104(2), 256–265. https://doi.org/10.1111/j.1360-0443.2008.02455.x on June 5, 2024



